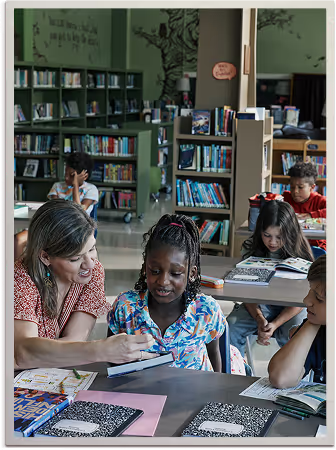
Health Equity startscloseto home.
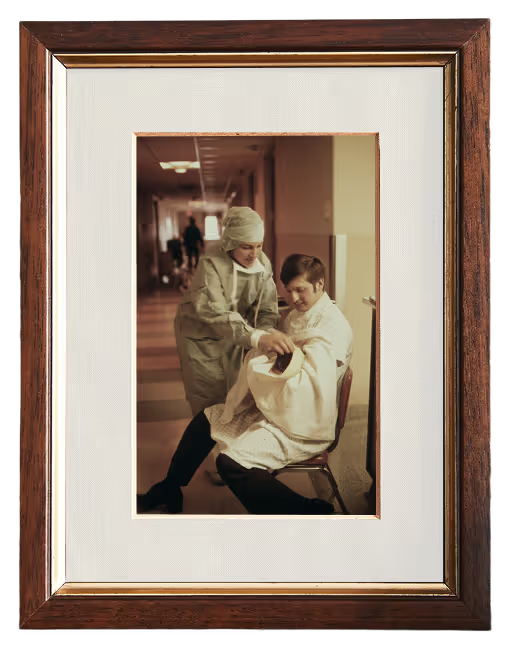
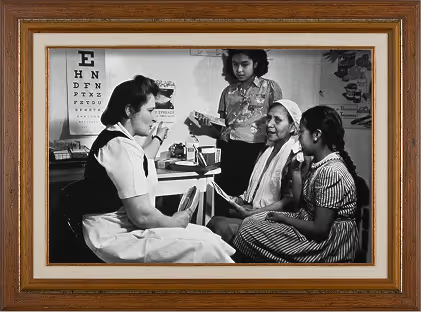
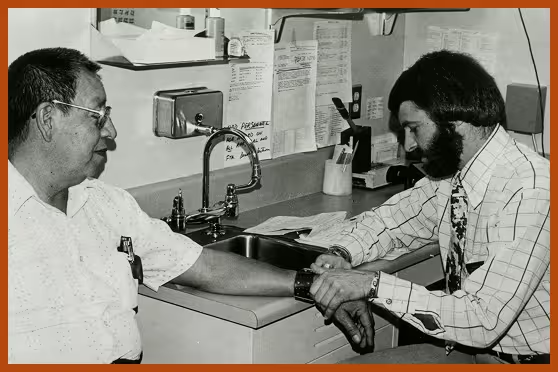
Across the nation, neighbors have always looked out for one another. But too many hardworking people—pursuing their dreams, raising families, serving their communities—are being left behind when it comes to health. Health equity means every American has a fair chance at good health, no matter their background or zipcode.
“Close to Home” is a place to understand these connections and build community, so good health is within reach for all.
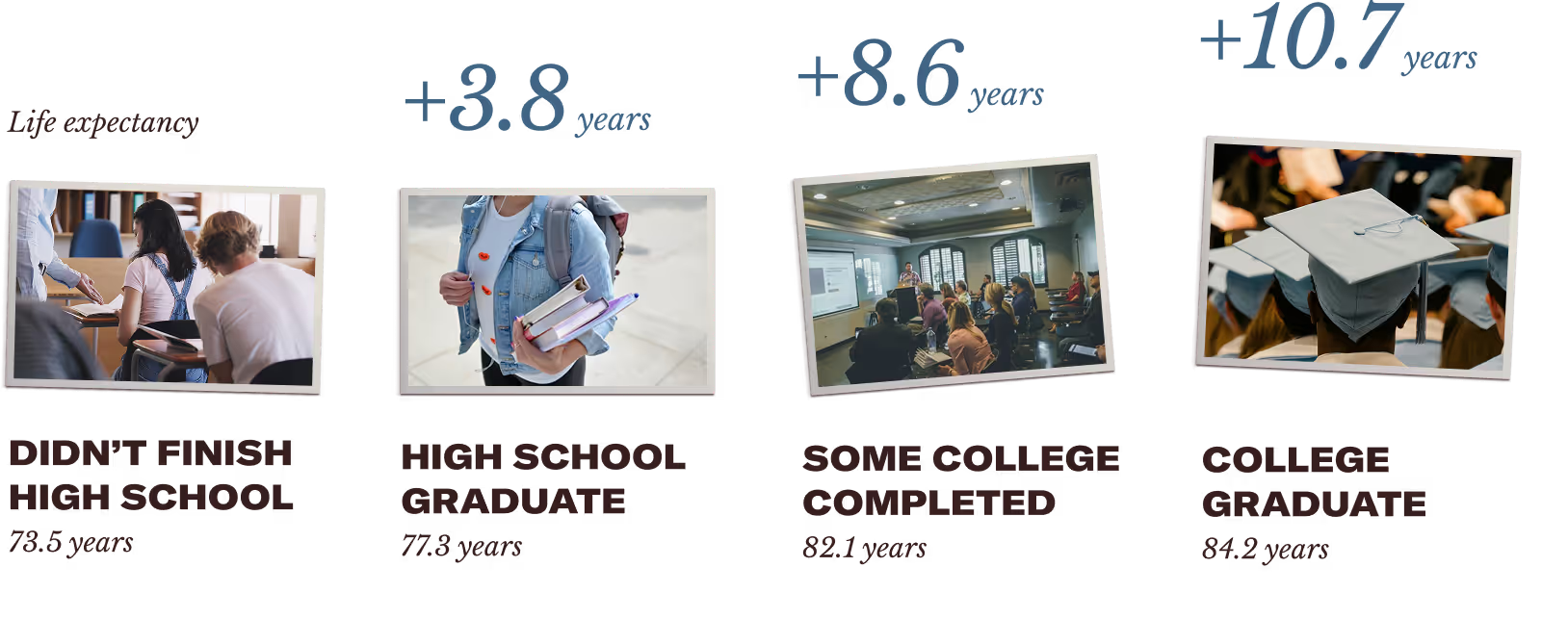
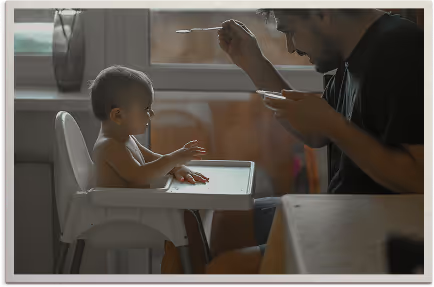
Our health is shaped by many factors—the places we call home, the work we do, the pressures we face, the food on our tables, and the support of our communities.
This diversity of lived experience should strengthen us, not limit our ability to lead healthy lives.



















Everyone's health story is different.


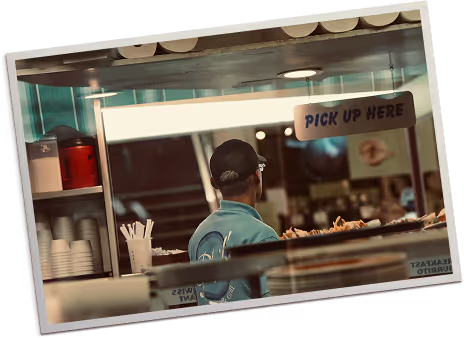
Across the country, hardworking people like Fred, Angela, and Marcus are doing their best, yet still face barriers that make staying healthy harder than it should be.
Their challenges aren’t a matter of effort—they reflect gaps in access that many families across America face every day.
Diversity, equity, and inclusion can help close that gap. Together, these values help ensure that every person in every community has the support and access they need.
Diversity
all people
Equity
fair access to the opportunities that help families stay well
Inclusion
everyone gets to be part of the American Dream
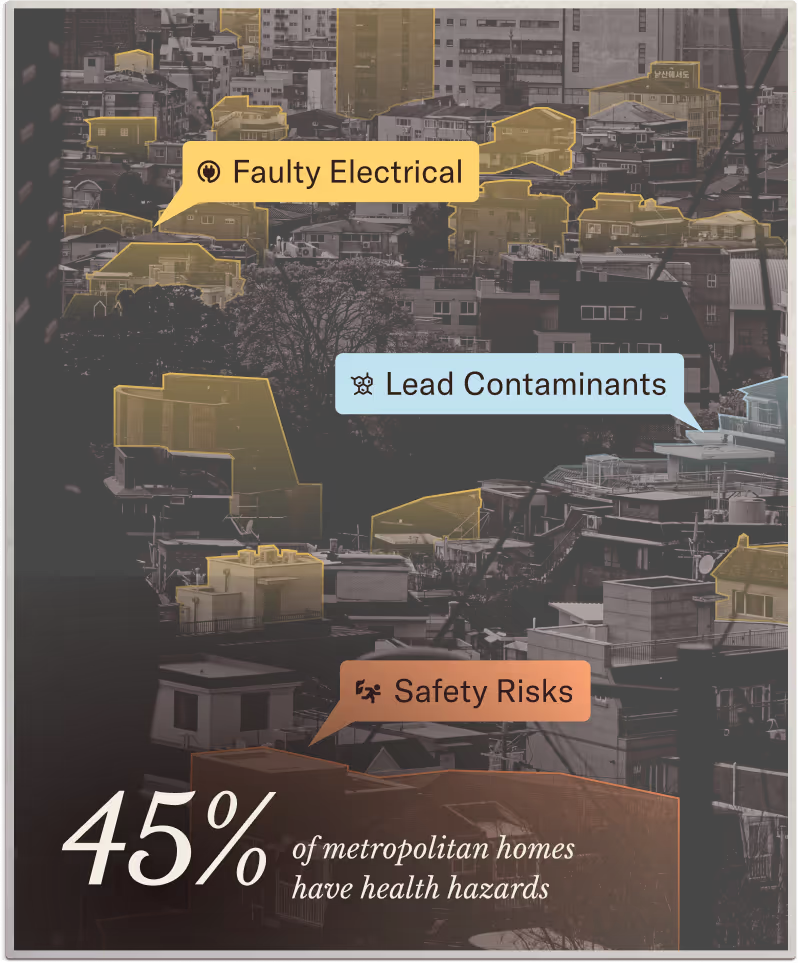
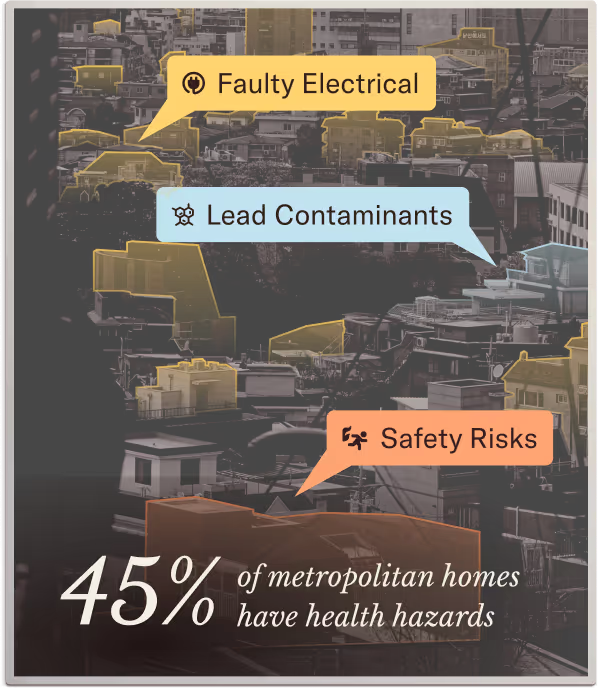
Our health depends on more than our individual decisions.
Health-related struggles can feel like bad luck or personal choices—but so much of what shapes our health comes down to the surroundings we share and the systems we all interact with.







Advancing Community-Driven Solutions for Health Equity
American Pride Rises
2026 Health Equity Microgrant Program
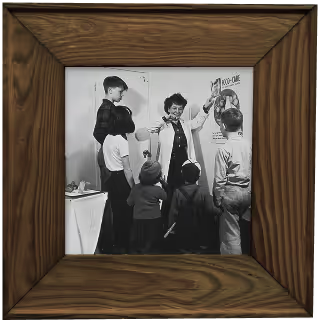
American Pride Rises (APR) is committed to building healthier, more equitable communities across the United States—particularly among populations that have historically faced barriers to health and opportunity. DEI is a critical lens through which we can tackle these disparities.
APR invites nonprofits and community-based organizations that are planning to or actively implementing projects aimed at addressing health inequities at the local level to apply for microgrants to support their efforts.



who can apply
Applicants
Must be U.S.-based nonprofits or community organizations with a fiscal sponsor.
Projects
Must be based in the US, align with the values of American Pride Rises, incorporate community involvement, and be focused on health equity.
APR welcomes all eligible organizations to apply and specifically encourages organizations led by or projects that empower:
Indigenous communities
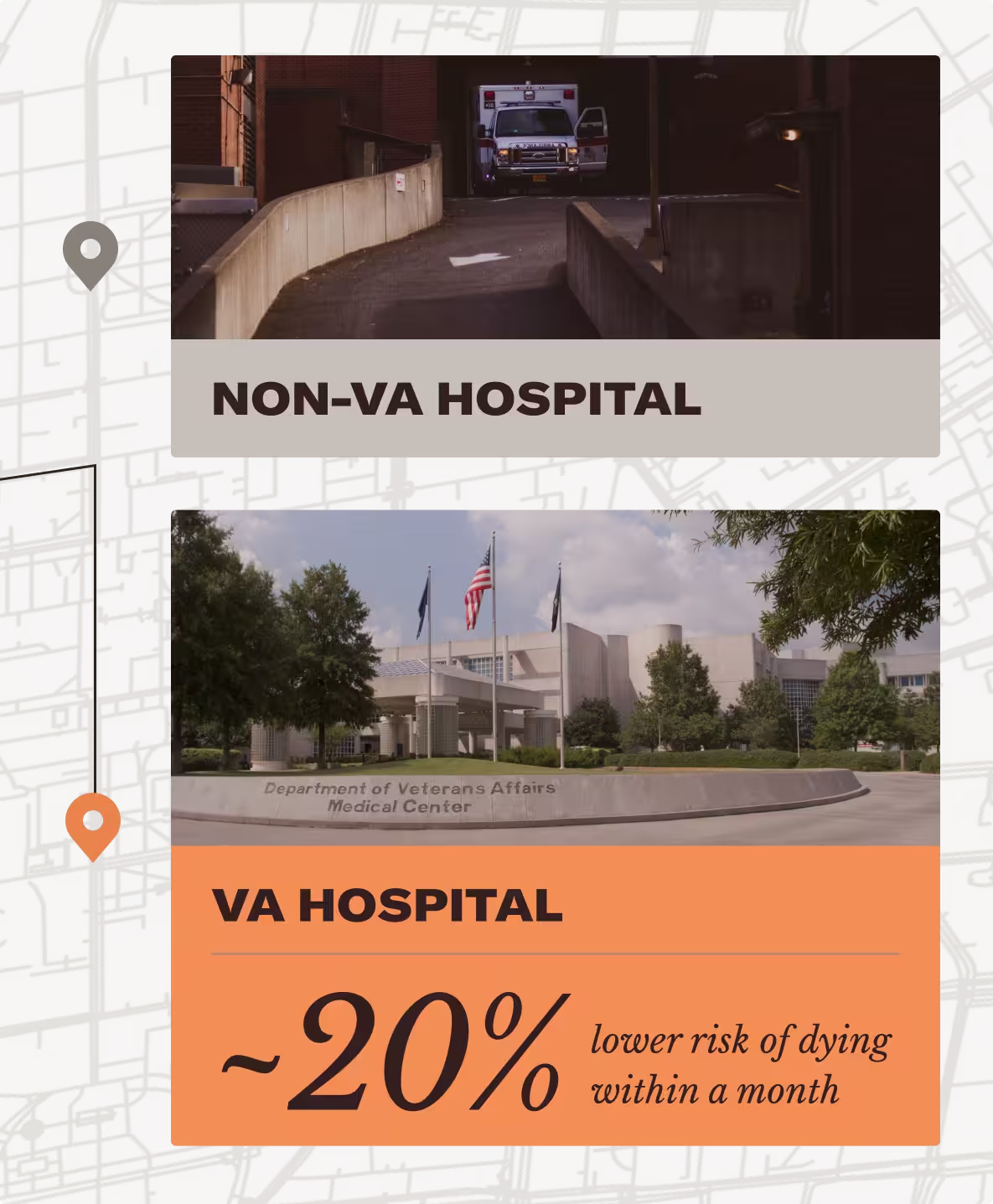
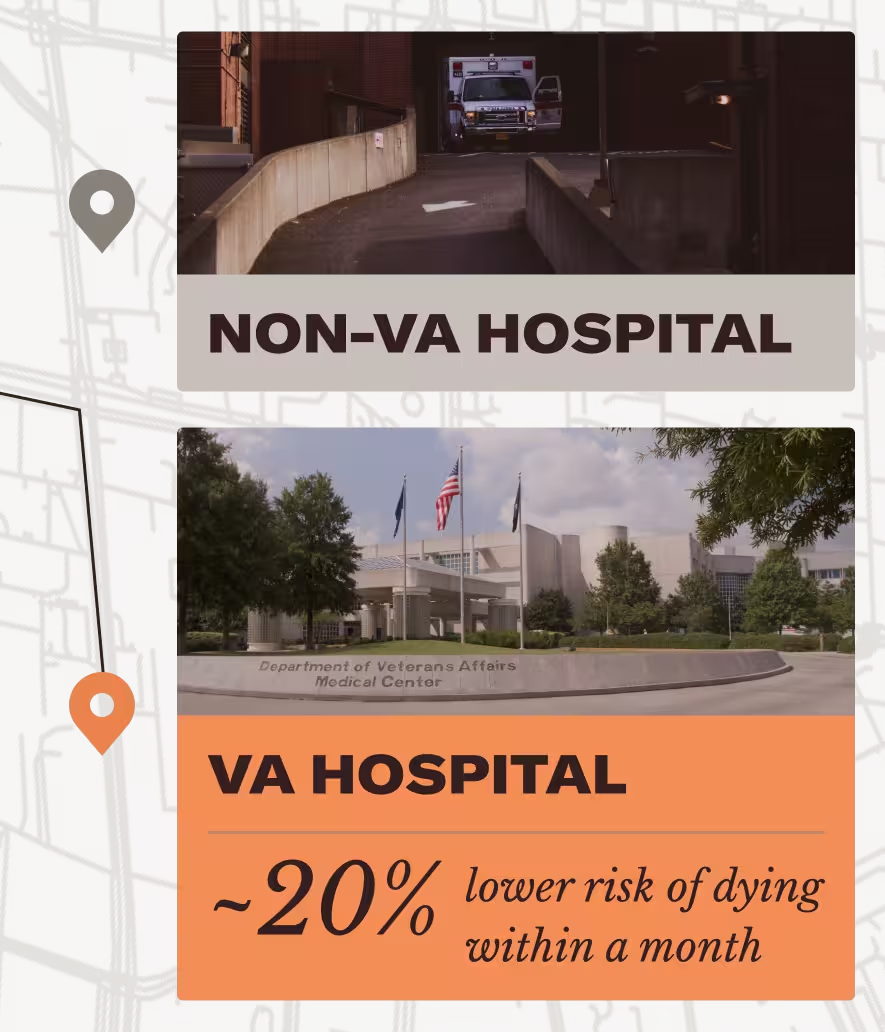
Veterans
Communities of Color
Rural communities
LGBTQ+ community
Disabled community
For this program, APR is especially interested in:
Projects demonstrating strong community engagement and leadership.
Efforts targeting specific populations that are disproportionately impacted by systemic health disparities.
Organizations located in or intentionally serving high-need regions.
Learnings that expand our understanding of how DEI supports and delivers improved outcomes.
Applicants are encouraged to think creatively about their project—bold and brave ideas are welcomed. Remember to keep the focus of the project aligned with health equity, but don’t be afraid to dream.
Timeline


funding tiers
I: Builder
Up to $5,000
For early-stage, foundational projects
II: Visionary
$5,000–$8,000
For scalable, forward-thinking projects
III: Dreamer
$8,000–$10,000
For bold, high-impact projects
How to apply
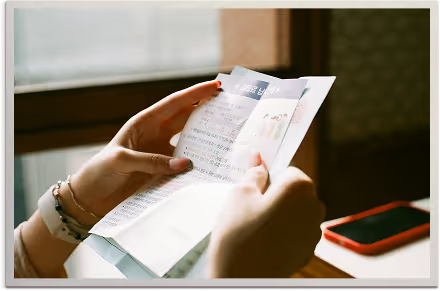
Applicants must submit an application including all required documents via APR’s online grant portal. Before submitting an application, please review application details and the outline of the microgrant program in the Grant Guide.
Questions?
Contact our Health Equity Team, grants@aprnetwork.org
Resources to take action close to home.
Ready to take action where it matters most? These resources offer simple, practical steps to support your family, show up for your neighbors, and strengthen your community. Together, we can build healthier, stronger communities—starting close to home.
Learn how fairness fuels healthier communities and what each of us can do right where we live.
Take real action to help your family, neighbors, and community thrive.
Spark conversations and mobilize your community to take meaningful action.
Taking care of each other is how we make good on the American promise.
We all deserve the chance to live healthy lives in the places we call home. As the threat to funding and coverage rollbacks continues to put access to health at risk, it’s up to us to stand up for ourselves and our neighbors.
Everyone has a role—whether you’re looking to take action, support your own well-being, or help neighbors and communities thrive. Learn more about what you can do to protect affordable healthcare for your communities and encourage your representatives to Just Fix It.
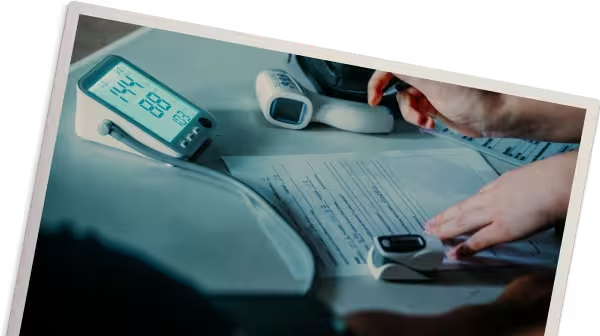
get to know the numbers
See how cuts will affect your costs. When coverage gets rolled back, families pay the price. Use the premium calculator or your renewal notice to see what rising costs could mean for your household. Understanding the real numbers helps you protect care close to home—before the burden grows.
Spread the Word
Show what’s really happening. Share your renewal notice, calculator results, or a quick post about rising costs. When neighbors see real numbers from real people, it builds urgency and strengthens the call to just fix it.
Take Action
Tell decision-makers to fix what’s breaking. Health shouldn’t depend on politics. Once you know what the cuts mean for you, send a message to your member of Congress. A quick email—with your real monthly costs—helps leaders understand the stakes and pushes them to protect funding, clinics, and coverage for your community.
Share Your Story
Your story matters, and by sharing your experiences, you’re helping to shed light on the real-world impact of medical expenses on individuals and families.
Together, we can make health accessible to all.


join us
As Medicaid and Medicare rollbacks grow, families are carrying more of the weight. Staying connected is how we protect each other and keep care close to home. Get updates, tools, and ways to protect care in your community.